|
Why does Morris Eye Group ask for my Medical insurance?
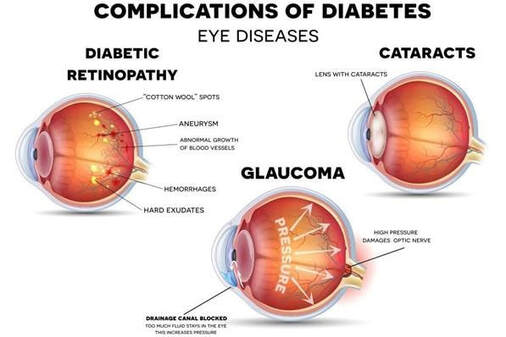
Morris Eye Group is a medical practice specializing in ophthalmology that diagnoses and treats medical conditions associated with the eye. Medical insurance generally covers eye care in relation to a medical condition. For example, if you need an eye exam because of cataracts, dry eyes, complications from diabetes, or in relation to diagnosed high blood pressure, then your medical insurance will provide coverage with ophthalmologist/optometrist. Medicare and other Medical Insurance Plans do cover the portion of the eye examination devoted to the determination of eye disease and the treatment of that disease. Medical plans also cover diagnostic testing to aid the doctor in diagnosing eye disease and monitoring its progress. If you have diagnostic testing performed, charges for these services will be billed to your medical insurance carrier. You will be responsible for any copays, coinsurance and medical deductibles associated with your specific insurance plans. Vision insurance covers the vision screening, a refraction which is the test performed to obtain a glasses prescription, including dilation, and benefits towards glasses/ contact lenses. Vision Insurance rarely covers diagnostic testing to diagnose eye disease or monitor its progress. If you need those services, their charges will be applied to your medical insurance plan, and any deductibles of coinsurance requirements of your medical insurance plan will apply. Vision Insurance typically covers an eye exam once every 12-24 months, depending on the plan. Medical Insurance can be used as frequently as the doctor deems necessary for monitoring any ocular Medical diagnosis. Why doesn’t my health insurance cover my eye glass prescription? Although eye refractions are an integral part of a comprehensive eye examination, they are specifically excluded from coverage by Medicare and most Medical Insurance Plans (HMO’s and PPO’s). Refractions are considered routine eye examinations for prescriptions for eyeglasses or contact lenses. Please see the CMS Publication “Your Medicare Benefits”. https://www.medicare.gov/coverage/eye-exams-routine Why are diagnostic pictures of my eyes not covered under my vision insurance? Vision insurance covers a once a year eye exam which includes; vision screening, a refraction which is the test performed to obtain a glasses prescription, dilation, and benefits towards glasses/ contact lenses. Think of this similar to benefits for an X-ray; photos are a diagnostic tool to assist the doctor in the treatment of eye conditions. If a patient has a medical condition and we take a photo, it is billed to their medical insurance. Do we accept all HMO plans? No. If you have an HMO you are assigned a medical group. A medical group determines which doctors you can see that are contracted with your particular health plan. We are only contracted with certain medical groups which is why we do not take all HMO plans. If you are unsure which medical group you are assigned to, we recommend calling your primary care provider. Here is a list of the medical groups we are contracted with: · Optum Care Network (OCN), previously known as Primary Care Associates (PCA) · Greater Tri-City · Scripps Coastal · Graybill · Perlman I have Medicare; why don’t they cover me 100% for my exam? Medicare has an annual deductible that must be met. Once that deductible is met, Medicare will cover the patient at 80% leaving a 20% responsibility for the patient. There are supplemental plans to Medicare that one can purchase to cover the portion that Medicare doesn’t cover. What’s the difference between Morris Eye Group and a Big Box Eye Care Center? Big box eye care centers only provide vision exams. Morris Eye Group is a full-service medical practice that provides medical diagnosis, treatment and surgical services including; cataract surgery, LASIK, glaucoma management and treatment, and corneal treatments. In addition to medical services, we have the largest optical dispensary in North County San Diego providing our patients with quality glasses and contact lenses. When a patient chooses to get full eye care with us, from start to finish, we have the ability to titrate any issues that arise after glasses have been dispensed because we monitor and control the process. If a patient elects to purchase eyewear elsewhere we have don’t have control on; materials/brand used, coding used, or how qualified the optician taking measurements. At Morris Eye Group, we use quality brands for our lenses and have access to choices for higher prescriptions, prism, and other brands should what we selected not work for the patient. Most of our opticians are licensed and certified and have a combined experience in optics of over 50 years.
106 Comments
You may have pink eye or another problem with your eyes. Here are the symptoms of Pink Eye: pink or red eyes, itchy, burning, watery eyes, a discharge coming from the eye (either white, yellow or green) and crusting along your eyelids that can even prevent your eyes from opening.
Pink Eye is also known as conjunctivitis and that can either be viral or bacterial. A viral infection is likely to start in one eye and spread to the other. If you are having a clear, watery discharge from your eyes and cold-like symptoms, you are likely having a viral infection. This infection will likely last 7-10 days. If it is a bacterial infection there may also be cold-like symptoms however, the notable difference is the thick (puss-like) discharge that forces your eyes to stick together. Bacterial pink eye lasts roughly 3-5 days and requires antibiotic eye drops to treat the infection. Pink Eye does spread very easily. The main action to prevent spreading pink eye is to wash your hands, whether you are the patient or you have a family member or friend with pink eye. If infected, avoid touching or rubbing your eyes. Avoid sharing personal items with other such as linen, pillow cases, towels, make-up or glasses. Most cases of viral pink eye do go away on their own, but you may need to be treated if you are in a lot of pain, noticing blurry vision or if you are sensitive to light. Bacterial pink eye should be treated by your eye doctor. If you are a contact lens wearer and you have pink eye, stop wearing your contact lenses till your treatment is complete or the symptoms have completely disappeared. Are you a contact lens wearer? You should always have a pair of back-up glasses with a current prescription for situations such as pink eye.  There is a new treatment for eyecare professionals to manage myopia progression. Made by Coopervision, MiSight is a daily disposable soft contact lens. It is the only method approved by the FDA to slow the progression of myopia in children (8-12 years of age at the initiation of treatment). Our very own Dr. Tan is one of the few optometrist certified to fit this lens that helps control myopia in children. Myopia, or nearsightedness, is an eye condition in which the eyeball elongates during development, thus causing blurry vision since the light rays focus in front of the retina (instead of correctly onto the retina). In 2010, 28% of the world’s population was myopic - by 2050, that number could reach 50%. With the growing myopia epidemic, there has been a greater need to slow down the progression of myopia. With higher myopia, there is a greater risk of developing other eye diseases such as glaucoma, retinal detachment, cataracts, and myopic maculopathy. Furthermore, the patient will also be more dependent on glasses and it may be more difficult to be a good candidate for refractive surgery. The increasing incidence of myopia can be attributed to a combination of two factors: genetics and environment. For genetics, even one parent with myopia increases the child’s chance of developing myopia by 3x, which can double to 6x if both parents are myopic. For the environment, research has shown that spending more time outdoors lowers the risk of progressive myopia. The earlier myopia management begins, the better the outcomes will be regarding the child’s overall eye health. Managing myopia starts with annual comprehensive eye exams. In the 3 year randomized clinical trial, the Misight lens decreased a child's average prescription from progressing by 59% and preserved a child's eye length by 52% versus the control lens. There were no adverse effects with contact lens wear and the kids found it comfortable to wear. Not only does Misight treat myopia progression, it corrects the child’s prescription and allows them to be independent of glasses (which is great for active patients). 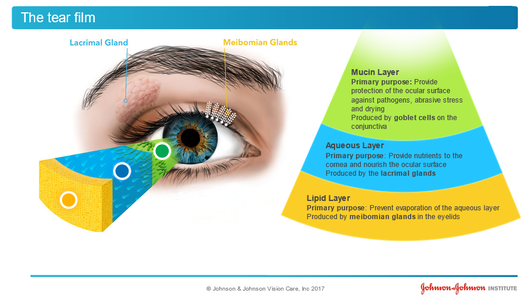 What is Dry Eye Disease? Dry Eye Disease or Meibomian Gland Dysfunction is much more commonly seen than in previous decades. Those that have it know its symptoms well: dryness, watery eyes, itchiness, stinging, burning, grittiness, redness, blurry vision and a foreign body sensation in the eye. The symptoms just don’t seem to go away and are very annoying. More than annoying, dry eyes can also produce chronic eye inflammation, corneal abrasions and corneal ulcers. Patients sometimes come in complaining that they have blurry vision and think they need new glasses when in fact, they have Dry Eye Disease that is disrupting their vision. Is it a simple problem to fix? Yes and No. Firstly, it requires an eye doctor to take a careful history, medical review of existing diseases and an eye examination. Correct Diagnosis of the cause is very important as it will dictate what treatments will work and what will not. If a patient has contact lenses that are not fit well, it may be a simple fix to change the contact lens prescription. How is Dry Eye Disease treated? Early treatment is the key to preventing irreversible damage to the glands of the eyes. The doctors of Morris Eye Group have a three- prong treatment plan with the goal to not just treat the symptoms but to treat the underlying cause. This necessitates a proper diagnosis of the underlying problem. Our doctors analyze the patient’s tear film quantity and quality. Are the eye glands producing proper lubrication to the eye or is the lubrication lacking enough essential oils to do the job? If the dry eye is a side-effect of a prescribed medication our doctors work with a patient’s primary care doctor or specialist to find an alternate medication to those that produce dry eyes. If a patient’s Meibomian glands are blocked the doctors prescribe a treatment to unblock them. There is also a home regimen to keep the glands open and a new Omega7 nutritional supplement that promotes the production of the oils that bathe the eye. We always recommend adding UV protection in prescribed eye wear. What causes Dry Eye Disease? The causes of Dry Eye Disease are varied and many. Here are the main causes: Aging, contact lens wear, autoimmune diseases such as Lupus, Sjorgen Syndrome and Thyroid Disease. Many prescribed drugs produce dry eye side-effects. We also know that computer, tablet and smart phone use have added to eye strain from their screen- emitted blue light. It is more common in females and in those that participate in outdoor sports such as golf, surfing and tennis. Dry Eye may also be due to an occupational exposure to known eye irritants. In some instances, over -the -counter eye drops to clear up red eyes actually make Dry Eye Disease worse. How does diabetes damage your eyes?
|
Encinitas Location |
Vista Location |
|
CA Open Payments | Privacy Policy | Accessibility | CA Privacy ©2024 Morris Eye Group Website by Medical Site Solutions |



 RSS Feed
RSS Feed


